Campylobacter
Campylobacter is a group of spiral-shaped bacteria that can cause disease in humans and animals. Campylobacter is one of the most common bacterial causes of diarrheal illness in the United States. Virtually all cases occur as isolated, sporadic events that are not typically associated with large foodborne outbreaks. Campylobacter jejuni, one of the most common strains, grows best at the body temperature of a bird, and seems to be well adapted to birds, which are frequently carriers.
Campylobacter is found throughout the world. Millions of Campylobacter cells can be released in a bowel movement from an infected person or animal. Campylobacter may be found in water sources such as private wells that have been contaminated with feces from infected people or animals. Human or animal waste can enter the water in many different ways (i.e., sewage overflows, polluted storm water runoff and agricultural runoff).
Campylobacter organisms have long been recognized as a cause of diarrhea in cattle and of septic abortion in both cattle and sheep, but they also are recognized as an important cause of human illness. Both Campylobacter fetus subspecies fetus (referred to then as Vibrio fetus) and C. jejuni were isolated from blood cultures of humans in the 1950s and at that time were thought to be rare and perhaps opportunistic pathogens.
Campylobacteriosis
Campylobacteriosis is a human Campylobacter-related infectious disease that can be passed to others. Symptoms can include diarrhea, cramping, abdominal pain, and fever within two to five days after exposure; some infected persons have no symptoms. Symptoms can also be accompanied by nausea and vomiting. Campylobacteriosis typically lasts one week. Although Campylobacter doesn’t commonly cause death, it has been estimated that approximately 76 people with Campylobacter infections may die each year.
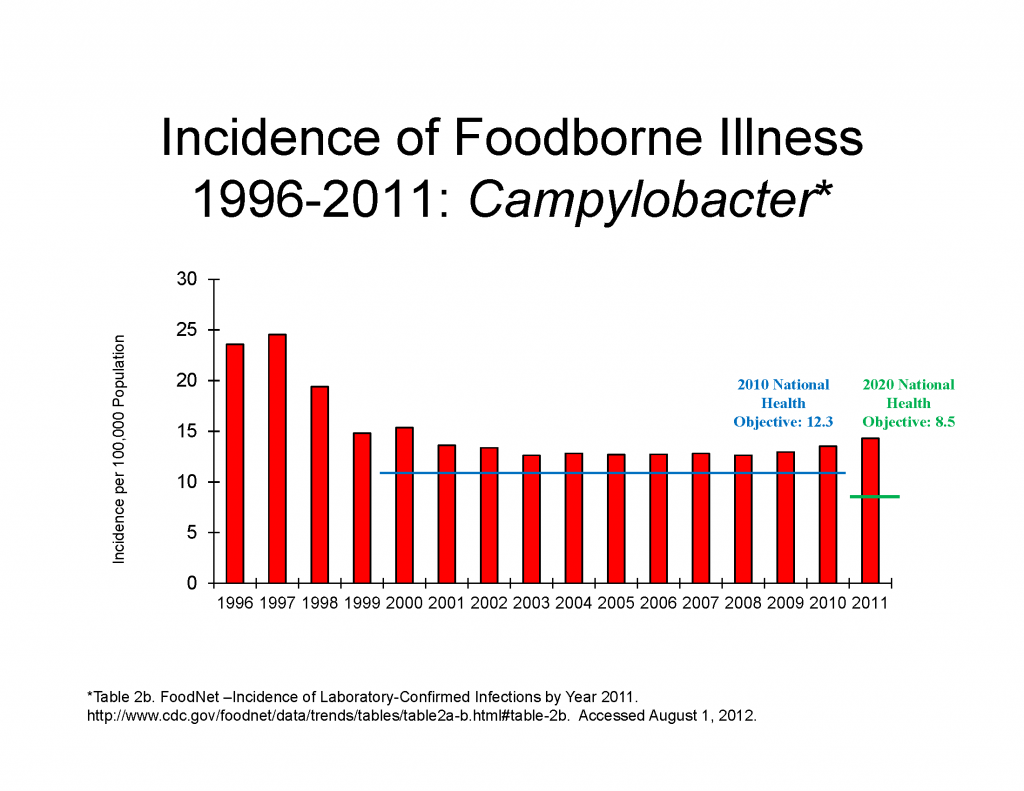
Campylobacteriosis occurs much more frequently in the summer months than in the winter. The organism is isolated from infants and young adults more frequently than from other age groups. Active surveillance through FoodNet indicates about 13.6 cases were diagnosed per 100,000 persons in 2010.
Some people may have arthritis following campylobacteriosis. Others may develop a rare disease that affects the nerves of the body beginning several weeks after the diarrheal illness called Guillain-Barré syndrome. Guillain-Barré syndrome occurs when a person’s immune system is “triggered” to attack the body’s own nerves, and can lead to paralysis that lasts several weeks and usually requires intensive care.
Larger outbreaks due to Campylobacter are not usually associated with raw poultry, but are usually related to drinking non-pasteurized milk or contaminated water. Animals can also be infected, and some people have acquired their infection from contact with the infected feces of an ill dog or cat.
Preventing campylobacteriosis
Most cases of campylobacteriosis are associated with handling raw poultry or eating raw or undercooked poultry meat. A very small number of Campylobacter organisms can cause illness in humans. Even one drop of liquid from raw chicken meat can infect a person, if Campylobacter is present.
One way to become infected is to cut poultry meat on a cutting board, and then use the unwashed cutting board or utensil to prepare vegetables or other raw or lightly cooked foods. Campylobacter organisms from the raw meat can then spread to the other foods. The organism is not usually spread from person to person, but this can happen if the infected person is a small child or is producing a large volume of diarrhea.
Incidence in meat and poultry
Campylobacter live in the intestines of healthy birds, and are associated with raw poultry. Many poultry flocks are infected with Campylobacter. It can be easily spread from bird to bird through a common water source or through contact with infected feces. Campylobacter is also present in the giblets, especially the liver.
Eating undercooked poultry, or other food that has been contaminated with juices from raw poultry is the most frequent source of this infection. Freezing reduces the number of Campylobacter bacteria present on raw meat as the microorganism is fragile. It also can be destroyed through drying and exposure to oxygen.
Government oversight
The Centers for Disease Control and Prevention (CDC) began a national surveillance program in 1982, to learn more about how Campylobacter causes disease and is spread. A more detailed active surveillance system was instituted in 1996, Emerging Infections Program Foodborne Diseases Active Surveillance Network (FoodNet); this provides more reliable estimates of disease occurrence.
Beginning in 1996, USDA’s Food Safety and Inspection Service (FSIS) implemented a new framework for meat and poultry inspection called HACCP (Hazard Analysis Critical Control Point). HACCP is a regulatory program that focuses attention on controlling food safety hazards at the most appropriate step or steps in the process. HACCP programs are designed to exert control over a variety of microbial pathogens, such as Campylobacter.
CDC is also making an effort to inform the public about campylobacteriosis and ways to avoid becoming infected. The Food and Drug Administration has produced the Model Food Code, which, if followed, could decrease the risk of contaminated poultry being served in food service establishments.
Advice for consumers
Cook all poultry products thoroughly. Make sure that the meat is cooked throughout and the inside is cooked to 165 F (74 C) using an instant read thermometer Wash hands with hot, soapy water before and after handling raw foods of animal origin.
Prevent cross-contamination in the kitchen by using separate cutting boards for foods of animal origin and other foods. Carefully clean all cutting boards, countertops and utensils with soap and hot water after preparing raw foods. Avoid consumption of non-pasteurized milk and untreated surface water. Make sure that persons with diarrhea, especially children, wash their hands carefully and frequently with soap to reduce the risk of spreading the infection. Wash hands with soap after having contact with pet feces.
Campylobacter can also be present in water, particularly well water. Heating water at a full boil for one minute (three minutes if you live in a high altitude) will kill Campylobacter. Boiled water should be stored in a clean container with a lid and refrigerated.
Helpful links
Third-Party Experts
Gary Acuff, Ph.D. Professor and Head, Department of Animal Science Texas A & M University (409) 845-4402 gacuff@tamu.edu
